Chronic Pain After Spinal Cord Injury
We take asprin for headaches, broken bones heal in six weeks, ongoing chronic pain however is a never ending nightmare of doctors drugs and treatments that typically yield little success and soon daily life becomes consumed by pain. From getting groceries to attending Susie’s wedding, life decisions are based on levels of pain felt today or of those percieved in time. So how can we ease and free ourselves from chronic pain with minimal drugs and little effort.
Training in the field of psychology I’ve been studying chronic pain more lately and noticed how deeply it is entrenched in lives watching someone close to me battle the condition. The very deadline I set myself for this article passed due to my relative’s chronic pain and her resulting difficulties. Whether you use a wheelchair, have ambulatory difficulties, or have other physical issues, the odds are chronic pain will factor in life at some point.
Who Suffers Chronic Pain

In developed countries, almost 20% of the adult population is currently afflicted with persistent and/or recurrent pain. According to International Association for the Study of Pain (IASP), only 1-2% of that documented chronic pain is attributed to cancer. The majority of that chronic pain is attributed to neck, back, joint, and musculoskeletal disorders.
There’s little wonder why people with on-going, unrelenting pain seriously consider suicide as an alternative to suffering a life defined by pain.
Only recently has the study and appropriate treatment of pain become part of mainstream medical research. Pain study now encompasses interdisciplinary research by psychologists, clinical doctors, biochemists, and neurophysiologists, among other professions. The most recent research has found that the sensations caused by severe, ongoing pain can literally change the chemical mechanisms within the central nervous system. Neuronal changes occur and the brain becomes primed to perceive pain, even after the source of pain is removed.
Additionally, research had found that pain perception is perceived differently based on gender and ethnicity. Believed to be attributed to neurochemical responses, women appear to experience pain far more than men, and those of African descent show a greater tendency to experience chronic pain than whites. When comparing responses to analgesic treatment to chronic pain, particularly various forms of opioids, men and women can expect markedly different levels of relief.
What is Chronic Pain
Pain is defined in three medical stages:
- 1. Acute pain lasts 30 days
- 2. Subacute pain spans 30 to 90 days
- 3. Pain that exceeds these time spans is classified as chronic pain.
Acute pain after any trauma or disease signals actual tissue damage as well as the potential for possible future tissue damage. Acute pain and chronic pain should be addressed and treated differently. The timing of pain treatment is another factor to consider, the longer someone experiences untreated pain, the longer it will take medical specialist to treat and hopefully remedy that pain.
Pain specialists note an individual experiencing severe pain treated within 60 to 80 days from onset, has a probability of becoming pain free near zero percent. If that same individual was treated within the first 30 to 60 days of onset, they would most likely have become pain free.
Economic Cost of Chronic Pain
Chronic pain left untreated or under treated drives the costs of health-care skyward in the form of visits to the emergency room, urgent care clinics, and predominantly extended stays in hospital. In the US alone, there are more than 50 million lost workdays related to persistent pain per year. Translated into cost for businesses $61.2 billion each year.
Cost Following Spinal Cord Injury
Chronic pain in persons with spinal cord injury (SCI) is a common and significant problem. Almost four out of five persons with SCI report chronic, persistent pain. Of that identified group, almost one-third report that chronic pain interferes with their daily activities and quality of life. In a separate study, over one third of participants with thoracic or lumbar SCI pain reported they were willing to trade recovery from their SCI for immediate pain relief.
Recent research has found that adequate pain relief around any spinal cord lesion early in treatment can help prevent later chronic pain. Correlations among those with incomplete spinal cord lesions where abnormal sensation exists near the initial lesion site treated for pain relative to the number who have gone on to suffer chronic pain later in life are also emerging in favor of early pain management.
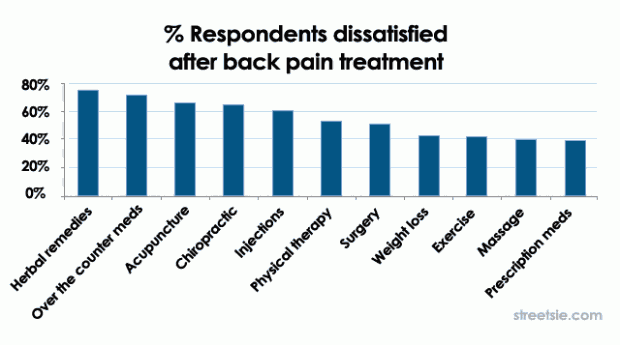
In a survey by Spinal Universe back pain treatments reported as most successful were also the most simple to enact, weight loss, exercise and massage, and furthermore aligned with other studies they conclude prescription pain management is the most effective in treating chronic pain.
Pain Management Narcotics and Addiction
There are numerous things to consider in the discussion of pain: how pain is measured, the sources of chronic pain, how individuals rate their pain, the perceptions of doctors, and the need of the sufferers, to name a few. However, based on my most recent experiences, the most difficult component of pain care is pain management through pharmaceutical treatments. I have found the single greatest fear, among untrained physicians and their desperate suffering patients, is addiction to narcotic pain relievers.
Despite our expectations to the contrary, chronic pain management is not explored in detail in medical school, unless one is going to specialize. The popularly held misconceptions regarding opiates, their derivatives, and the newer non-opioid analgesics are one of the major reasons many suffer chronic pain needlessly. While studying psychology, my primary focus was substance abuse, a field which is complicated and filled with emotional issues.
There is a clear and well-defined line between an individual whose body has sustained trauma seeking pain relief and substance abuse. The concepts of addiction are complicated and fraught with different theories of addiction and treatment. To clearly examine the nomenclature of abuse and addiction to medicinal drugs intended to relieve pain we need to understand that profound differences exist between medical pain relief, substance abuse, and chemical dependence.

Substance abuse is defined as the use of drugs or any other chemical substance (legal or illegal) with some pattern of regularity, such as drinking to excess every weekend. Substance abusers are still able to maintain their life roles and responsibilities with some degree of competence. Monday is still a work day and the individual arrives on time, worn out and hung over, but still at work.
Chemically dependent individuals are, however, a completely different story. Chemically dependent individuals devote all their attention, emotions, and thoughts toward every aspect of their addicted life. A chemically dependent person chooses to forgo relationships with their family and friends; their primary relationship is with their drug of choice. Their life revolves around the drug, instead of enhancing quality of life, it consumes their life. It’s rare for a person who is adequately treated for chronic pain to display such behaviours.
While at times chronic pain may seem to overshadows everything in our lives, it is not by choice. When we seek treatment and care for chronic pain, we are entitled to the most appropriate medication possible, whether that is morphine or methadone. When we experience such profound chronic pain, the odds are very slim that we will become addicted to our medication. Unless there is a history of addiction in the family background, it is relatively safe to take powerful medications, strictly according to the prescriber’s orders.
Making changes and adjustments to narcotic pain medication is reckless and potentially life threatening, unless under the prescriber’s orders. If at any time you feel you have become dependent on pain medication consult your physician and ask they re-examine your prescriptions and drug regime.
Conclusions
Chronic pain is frustrating and exhausting. It hurts those who suffer from it and those who love and care for them. Chronic pain is a condition that is often extremely difficult to treat. It can take months or even years to find the right physician, the right treatment, and the right medication. Many find it difficult to stand up to a doctor and tell them we are capable of participating in the choice of our treatment, particularly if narcotics are part of the discussion.
We are all well within our rights to educate ourselves and subsequently advocate for ourselves or a loved one. We are all entitled to pain relief and an improvement in the quality of life. The consequences of inadequate chronic pain relief are potential greater harm than the consequences of addiction. The earlier a possible dependency is addressed the more effectively it can be dealt with. If you have concerns or questions about chronic pain, please contact your physician.
Resources
- ABC of Spinal Cord Injury, 4th Edition; Grundy, David (ed). 2002, BMJ Books, London.
- American Pain Foundation; http://painfoundation.org
- Encyclopedia of Disability; Albrecht, Gary L. (ed). 2006, Sage Publications, Thousand Oaks.
- Fundamentals of Substance Abuse Practice; Johnson, Jerry. 2004, Brooks/Cole-Thomson Learning, Belmont, CA.
- Health.Com; http://www.health.com
- International Association for the Study of Pain; http://www.iasp-pain.org
I am a T-12 complete after being run-over by some nitwit in an SUV while driving under “road rage”. He got a $300.00 ticket, I got a wheelchair for life.
The pain is so bad sometimes for the first time since my accident (Dec ’06) I’ve contemplated suicide. But that’s out of the quesiton, since I’m a husband and father, and the major bread-winner.
I have a litany of hard drugs I take with no effect, it seems the only way to “get away” from the pain is to immerse myself in something like writing, working on antique motors, or excercising. I work full time, and that helps as well.
So to all you paralyzed people out there with cronic nerve pain, don’t give up, get involved in something, and kick those narcotics!
Good luck,
Matt Cuddy
Burbank, CA
I’ve had severe chronic pain for over a decade. Caused by vitamin and mineral deficiencies, and also spinal injury.
Here’s a list of things that have helped as much as my morphine:
1) Transdermal Magnesium Chloride for pain relief.
Also Zinc Chloride. Basically, any vitamin or mineral that you’re deficient in can help reduce pain. That’s been my experience.
Google your symptoms + mineral/vitamin deficiency symptoms. I’ve had more success than my doctors. Just got to be cautious and start on a low dose of whatever you’re trying out.
2) Magnets, buy your own strong ones and attach to clothing using a second magnet (place one on either side of clothing in vicinity of pain)
I put the south pole against my skin, it seems relaxing. North pole stimulating.
3) Heat heat heat, and/or cold. Never underestimate how powerful heat or cold can be. I use hot water bottles year round.
4) Massaging oils into the skin. Even olive oil can help. But Eve primrose and hemp seem better.
5) Oral cannabis works far better for physical pain than smoking.
6) Smoking constricts (closes) your blood vessels, so go smoke free or at least reduce it. When you get down to one or two a day, you’ll notice how much worse you feel physically after a smoke. That will help you cut down further.
7) Essential oils such as Lavendar, Rose, Orange, Peppermint etc. can help relaxation and are pleasurable to use. A little goes a long long way. Add a drop to the collar or cuff of old clothing and inhale at intervals. Or a few drops on a clean hankerchief/rag.
Use in baths and showers, on bed clothes, you name it. Just be careful to test for staining first. Some oils are actually more like water, others are really oily and will stain.
8) Binaural beats. Try them for free on Youtube with a pair of headphones (you dont need high quality headphones. Your ears and brain just need to be able to hear the slight difference between the tone going into your left ear, and the tone going into your right. So stereo hearing is more important than expensive headphones).
9) Exercise. Difficult if you’re often bed bound. Google bed Yoga or if you’re lucky, and have a helper, they can move your limbs/body for you.
Hi. My friend is a t 5/6 complete paraplegic after a motor bike accident 18 months ago he has 7/10 pain constantly he is on a heap of narcotics that seem to be doing sweet fa we have tried massage heat pack oils vitamin sups with no relief he has a baclofen pump which has stopped spasms 98% and now their talking Adding morphine or anesthetic anyone out there tried this or any other solutions its wrecking his life oh he’s also used pot to no avail. Really need some help with this one. Thanks sue oh and I love this web site its great to read and get informed from people in the dame position
I just wanted to add a quick update to this thread. Have any of you with chronic pain or spasms had a medtronic pump implanted? Chris had his trial and his pain went to a 3! He then had the pump implanted and just recently had it filled the first time. It will continuously supply pain meds at a set rate 24/7 and can be programmed to allow a higher dose for break through pain. It will take approx 3 visits to achieve efficient delivery but it has been a game changer as pain will be reduced, made manageable, and oral narcotics, patches, etc will be discontinued. Is anyone else having success with this?